 Tonya introduces herself as “an Army veteran and chronic illness warrior.” She has needed all of the skills, determination, and mental toughness of a warrior to battle a disease that went undiagnosed for a staggering 17 years and now makes it impossible for her to eat and digest food.
Tonya introduces herself as “an Army veteran and chronic illness warrior.” She has needed all of the skills, determination, and mental toughness of a warrior to battle a disease that went undiagnosed for a staggering 17 years and now makes it impossible for her to eat and digest food.
Her response to all the difficulties she has faced is to reach out to educate others about gastroparesis, a condition that disrupts the ability of muscles in the stomach to push food through the digestive tract.
While the direct cause of gastroparesis is unknown, Tonya can track the start of her health problems to her service in the Gulf War.
Tonya’s Army unit was deployed to Saudi Arabia in 1995. In addition to her work as a signal support systems specialist keeping communication lines operational, she frequently marched in the color guard, presenting the American flag in the desert heat. She didn’t see combat but was exposed to all the toxic fumes of war for six months.
It is estimated that nearly one-third of all who served in the Gulf War developed unexplained chronic symptoms, including gastrointestinal and digestive issues. The Veterans Administration has determined that Tonya suffers from what is now called Gulf War Illness.
Tonya felt fine and had no “stomach issues” when her unit first returned home. Standing at 5’ 8 ½” and weighing 191 pounds, Tonya went on a weight loss program and successfully dropped to 175 pounds.
Then the good news stopped. She began getting stomach pains and felt constipated. Soon she had bouts of nausea and vomiting. “I would go to Sick Call and be told, ‘Oh, you just have a virus. Here are some meds; it will pass’,” recalls Tonya. But it didn’t. The discomfort, pain, and vomiting continued, and so did the weight loss.
After four years of service, Tonya decided to leave the Army, but her symptoms only worsened in civilian life. The doctors she saw at the VA hospital only treated her symptoms. It wasn’t until 2013 that she was given a gastric emptying study.
“The doctor didn’t expect the study to show much and said I would hear the results later in the week. That same day he called and told me I had severe gastroparesis and immediately started me on Reglan,” said Tonya.
This standard gastroparesis medication, however, provided only short-term relief for Tonya. After 18 months, she began vomiting again, and her weight dropped to 120 pounds.
It was her own online research that led Tonya to civilian gastroenterologists in Houston and then San Antonio, who could tackle her complex condition. After medications and diet modifications failed, a gastric stimulator was implanted in her stomach. This sophisticated electronic device proved helpful for less than two years. Then it, too, stopped relieving her symptoms.
At this point, Tonya had a feeding tube placed and had the help of a dedicated dietitian at the VA to find the proper enteral nutrition formula. “I had the tube for two years. We tried multiple formulas, but nothing fully worked. I wasn’t absorbing enough calories, and I kept losing weight. I was down to 112 pounds.” says Tonya.
Her dietitian and gastroenterologist then recommended home parenteral nutrition (HPN).
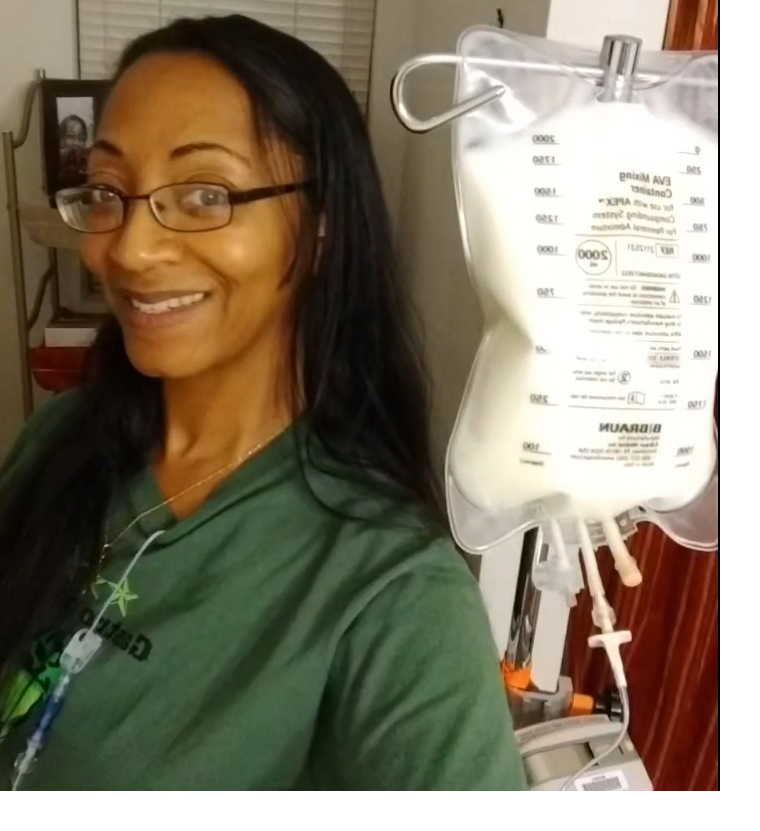
Tonya quickly took command of her own care. “Once the nurse came to my home and showed me how to set up HPN and access my port, and I showed her I could do it, I was on my own. I prefer to be self-sufficient and do it the way I like it,” Tonya affirms.
Her advice to others getting HPN is straightforward. “If you take it step-by-step, it’s easy. All you have to do is this, then this, then this. You’ve got to have a schedule and then stick with it,” she advises.
Tonya is on HPN for 12 hours a day. She prefers to take it overnight, so she is free the next day for any appointments. “That way, I don’t have a bag to deal with. There’s always the question of where to put the bag,” laughs Tonya.
Her home infusion dietitian and physician work closely together and review her bloodwork every week. So far, her nutrition formula is working well. She currently weighs 143 pounds.
Tonya now devotes her time and whatever energy she has to communicating with other chronic illness warriors and advocating for healthcare information and access.
She is an active contributor to numerous online support groups, including the Texas and national gastroparesis groups as well as tube feeding and HPN groups. She is also an Ambassador for the Oley Foundation, which works to enrich the lives of those living with home IV nutrition or tube feeding.
“When you have a chronic illness, it helps if you can go online and find someone you can relate to. You’ve not met them, but you form all these bonds. There are 10 to 12 people I message every day. Even a short ‘How are you doing?’ or a ‘Not heard from you, you OK?’ can mean a lot.”
Tonya has also raised her strong and clear voice to persuade two different mayors of Killeen, TX to officially recognize Gastroparesis Awareness Month in August. She has also shared her story and struggles with the local newspaper and a TV station to help educate her community about this little-known disease.

Mayor Debbie Nash-King (second from left) presenting Tonya (third from left) and friends with a Gastroparesis Awareness Month proclamation.

Tonya in a 2018 interview with KCEN during Gastroparesis Awareness Month.
“I started advocating because I was tired of doctors not always giving me the full picture of what could be done and the treatments that were out there. I want to impact change in my local area as well as nationwide,” Tonya wrote in a
recent blog. “The only way change will happen is when we start doing things to make it occur.”
Tonya is making every day—and every calorie she is receiving—count.
|
Getting and Giving Support
The Oley Foundation, a home nutrition support community and advocacy group, provides a number of ways for patients, families, and caregivers to connect for information and support, including:
- A
chat forum for peer support and community discussions
-
Support groups for adults, teens, and school-aged-kids
-
Oley Ambassadors across the U.S. and Canada who can be reached online, by phone, or in person
|
|
Every Voice Counts!
Help advocate for clinical nutrition care at
nutritioncare.org/takeaction. Join ASPEN in supporting federal legislation to:
- Improve the quality and safety of nutrition support.
- Ensure fair reimbursement for nutrition support care.
- Preserve patient access to home infusion.
Spread the Word on Malnutrition
Support ASPEN’s Malnutrition Awareness WeekTM. This annual campaign helps educate healthcare professionals and consumers on the detection, intervention, and treatment of malnutrition. Visit
nutritioncare.org/maw.
You can help by:
- Asking your governor or mayor to proclaim Malnutrition Awareness Week. This year, it’s September 18–22.
- Contacting your local media with story ideas.
- Participating in Malnutrition Awareness Week activities.
|
Read more patient stories.