 John Place makes it his business to give people happy memories.
John Place makes it his business to give people happy memories.
Since 2012, this affable and energetic entrepreneur has brought his Fun Photo Booth Parties to weddings, corporate events, birthdays, bar mitzvahs, and a host of other celebrations and gatherings throughout Miami and Broward County, Florida.
Then the COVID-19 pandemic shut down the parties and his business. In June, the virus would also shut down his memory.
“The last thing I remember is Father’s Day, June 21,” says John. He recalls not feeling well and having a high fever. Then things got fuzzy. “People tell me I was talking with them on the phone, but I can’t tell you what was said.”
His wife, Michelle Zymet, can’t forget the next four days of uncertainty and concern as John’s high fever persisted, then coughing, shortness of breath, and a dash to the hospital.
“It was a whirlwind of emotions … from shock and concern to chaos and fear. It was a nightmare. All of my focus was on John and trying to do anything possible to save his life!”
John was admitted to Westside Regional Medical Center, a 224-bed hospital in his hometown of Plantation, Florida, where it was confirmed that he had contracted COVID-19 and pneumonia and had undiagnosed diabetes and high blood pressure.
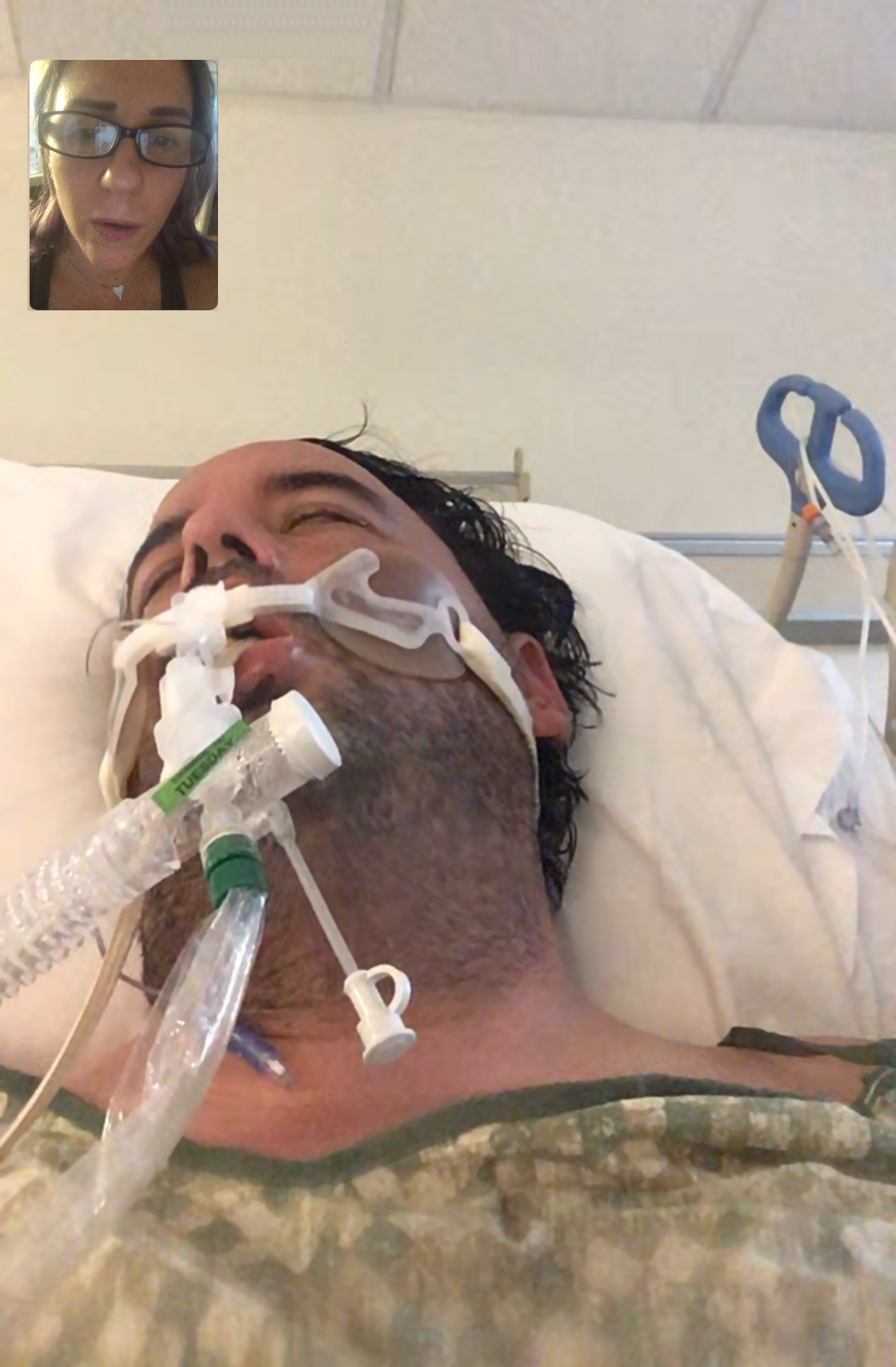 On June 29, his fever persisted, and his breathing further declined. He was moved to the ICU and placed on a ventilator to help with his breathing.
On June 29, his fever persisted, and his breathing further declined. He was moved to the ICU and placed on a ventilator to help with his breathing.
To provide the nutrients and energy his body needed to fight the virus, an orogastric tube was inserted into his mouth, through the esophagus, and into the stomach.
John’s nutrition support was complicated by his uncontrolled diabetes. Special diabetic formulas fed through the tube were used to first lower and then maintain his blood sugar levels, as well as deliver all of the protein, carbohydrates, fat, vitamins, and minerals his body desperately needed.
For 20 days, the ventilator and orogastric tube kept John alive and gave him the time to be treated with plasma infusions, steroids, and a 10-day course of the drug, remdesivir.
To ease his breathing, John was periodically turned from lying on his back to lying on his stomach. “They preferred to have him on his back because it was easier to give him the nutrition he needed,” recalls Michelle.
To keep him connected with his wife and three children, the nursing staff would FaceTime with his family and hold the phone to John’s ear.
“We were able to tell him how much we loved him and encouraged him to keep fighting. We had no way of knowing for sure, but we were hopeful he could hear us,” says Michelle, who is a strong believer in prayer and positive thinking.
After a number of ups and downs, John’s overall condition steadily improved, and on July 15, he was removed from the ventilator. All who know him were very grateful that he was alive, awake, and able to celebrate his 43rd birthday in the ICU.
An indicator of just how much energy it takes to fight a disease, John lost 49 pounds in less than a month. It took some time before he would be able to eat on his own. His medical team first had to be sure he could swallow after being on a ventilator for weeks.
“They gave me a graham cracker and asked me to chew and then swallow it. I couldn’t do it,” sighs John. “Luckily, I passed the swallow test the next day.”
The first of numerous calls and consultations from the dietitian quickly followed. “They didn’t waste any time giving me literature on diabetes and sample menus, and teaching me about portion control and carbohydrate point exchanges. I had a little trouble with the points but got the message about the importance of a balanced diet right away.”
His understanding and optimism grew as the special diabetic meals ordered by the dietitian arrived at his bedside. He especially looked forward to the nutritional supplement that was included on his food tray. “I can handle this,” concluded this go-getter.
 John should have no problem recalling August 6. That’s the day he was released from the hospital and sent home into the loving care of his family. Of course, John didn’t leave the hospital quietly. It was a memorable moment with a cheering crowd, balloons, flowers, and custom-made t-shirts proclaiming “I’m Alive.”
John should have no problem recalling August 6. That’s the day he was released from the hospital and sent home into the loving care of his family. Of course, John didn’t leave the hospital quietly. It was a memorable moment with a cheering crowd, balloons, flowers, and custom-made t-shirts proclaiming “I’m Alive.”
While John is very grateful to be alive and optimistic about his future, this unique and unpredictable virus left him unable to fully extend and use his right arm, and he has some muscle problems on his left side.
He faces a long and unknown road to recovery. It will take time to literally get him back on his feet and hopefully regain full use of his arm. “I now have a flat stomach,” he says with a laugh, though he’s not so happy with “muscles that hang like turkey gobblers.”
“I was lucky,” affirms John. “Right hospital. Right treatment. I can’t say thank you enough to the hospital staff. They worked so very hard. I couldn’t believe how much gear they had to put on—gowns and masks and two layers of gloves—just to come into my room. They’re incredible.”
His wife echoes his gratitude for all the hospital staff’s skill and efforts, and adds her thanks for their support and their time and patience relaying test results and educating her on her husband’s status.
John agreed to share his personal experience as he sees it as a cautionary tale.
Before the virus struck, he had some suspicions about his health. He knew he was overweight and had been drinking a lot of juice and going to the bathroom frequently. His body was telling him something wasn’t right, but he just didn’t pay enough attention.
His story also made the news, particularly in Florida, because John believes he caught the virus from his 21-year-old son who broke the family’s stay-at-home policy for an unmasked visit with some friends. All five members of his family tested positive for COVID-19, but only John became seriously ill.
Unfortunately, there are countless similar stories.
ASPEN has a number of useful nutritional guides for both those who have been hospitalized with COVID-19 and those treated at home. They are available at nutritioncare.org/COVID19.
Read more patient stories.