Enteral nutrition (EN), also called “tube feeding,” is a way of providing nutrition directly into the gastrointestinal (GI) tract through an enteral access device (feeding tube) that is placed with its tip in the stomach or small intestine. Enteral nutrition is a special liquid food mixture containing all of the nutrients required to meet nutrition needs, such as protein, carbohydrates, fats, vitamins, minerals, and other nutrients. The formula can include ready-to-feed liquids, formulas made from a powder or a concentrate, or can be blenderized food. Blenderized formulas may be home-blended or commercially prepared. For babies, human breast milk or infant formula can be considered EN when given through a feeding tube.
 What is an enteral access device (feeding tube)?
What is an enteral access device (feeding tube)?
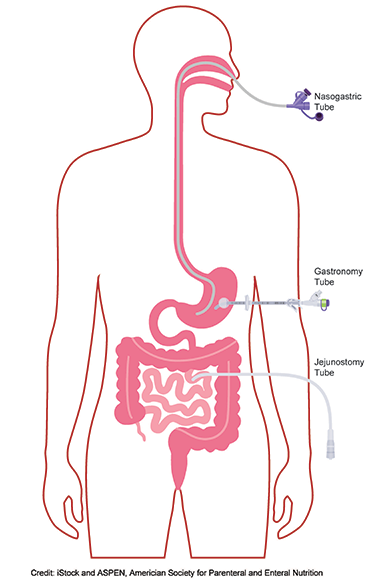
Enteral nutrition is administered through an enteral access device, also called a feeding tube. There are several types of feeding tubes:
- Tubes placed through the nose into the stomach (nasogastric) or the small intestine (nasoduodenal/nasojejunal). These tubes are called nasoenteral tubes.
- Tubes placed through the mouth into the stomach (orogastric) or the small intestine (oroduodenal/orojejunal). These tubes are called oroenteral tubes.
- Tubes placed directly through the skin into the stomach (gastrostomy) or small intestine (jejunostomy)
Your healthcare provider and/or nutrition support team will discuss the different types of enteral access devices and determine what is best for you based on your unique clinical scenario.
Who can receive EN?
Patients of all ages (neonates, infants, children, adolescents, and adults) can receive EN. Thousands of patients receive tube feeding yearly in acute care settings, and many continue EN at home or in long-term care facilities.
When is EN indicated?
Enteral nutrition is indicated in patients who cannot take any or enough nutrition by mouth. This may happen when that person has cancer, critical illness, gastrointestinal (GI), or non-GI diseases such as stroke, kidney disease, or lung disease.
What are the primary benefits of EN?
Enteral nutrition provides the nutrients required when a patient cannot consume enough food or nutrients needed to maintain health or recover from a disease, illness, or condition. Patients can become malnourished without proper nutrition and develop adverse conditions such as infections or even death. Enteral nutrition helps maintain normal digestion and absorption of nutrients through the GI tract, which are necessary for proper body functions and overall well-being. Enteral nutrition can help treat malnutrition and supports the immune system and thus is associated with reduced infections. Enteral nutrition can also prevent the development of malnutrition.
Are there side effects of EN?
Although EN is generally well tolerated, it may be associated with a few side effects. Side effects may include GI-related (e.g., nausea, vomiting, diarrhea, abdominal distention, constipation) and metabolic issues (e.g., electrolyte and mineral imbalances, fluid imbalance, and glucose intolerance). It is important to note that many of these side effects can be prevented or managed with appropriate monitoring.
How long does a person require EN?
Patients may be on EN briefly for a few days or weeks in the hospital to carry them over until they can meet nutrition needs by mouth. In other cases, EN is used lifelong. It is dependent on a patient’s clinical conditions. Patients can live well on EN for as long as needed.
How is EN administered?
Enteral nutrition is administered through the enteral access device using a syringe, container, or bag with a gravity feeding set or via a feeding pump. Enteral nutrition can be administered continuously or intermittently. When at home, the EN can be delivered any of the above ways, but when using a feeding pump, EN can be administered over 24 hours (continuously) or over a shorter time, such as 10-18 hours (cycling).
What does EN's follow-up care and monitoring entail (e.g., medical team, patient/home healthcare, and dietitian care)?
If a person goes home on EN, follow-up appointments with a healthcare provider and NSPs will be scheduled. At these visits, weight and nutrition status will be monitored to determine if adjustments are needed in the EN regimen. Sometimes, a home care nurse or dietitian will schedule home visits for additional follow-up monitoring.
Disclaimer: This content has been developed for use by healthcare professionals to inform other clinicians and/or patients/caregivers. ASPEN is making this content available for informational purposes only. This content is not based on ASPEN Board Approved documents and should not be confused with ASPEN clinical guidelines as it was not developed according to ASPEN guideline processes. Recommendations provided here do not constitute medical or other professional advice and should not be taken as such. To the extent that the information presented here may be used to assist in the care of patients, the primary component of quality medical care is the result of the professional judgment of the healthcare professionals providing care. The information presented here is not a substitute for the exercise of professional judgment by healthcare professionals. Circumstances and patient specifics in clinical settings may require actions different from those recommended in this document; in those cases, the judgment of the treating professional should prevail. Use of this information does not in any way guarantee any specific benefit in outcome or survival. This tool is intended to supplement, but not replace, professional training and judgment.